As healthcare professionals, we get bombarded with seemingly endless compliance training requirements on top of our patient care duties.
From information governance to health and safety, the sheer volume of required modules can feel daunting.
This guide will clearly define “statutory” versus “mandatory” requirements, explain common topics, provide learning tips, and most importantly, discuss how these two training requirements ultimately aim to protect us and our patients.
Together we’ll make sense of these learning obligations in service of providing safer, higher quality care.
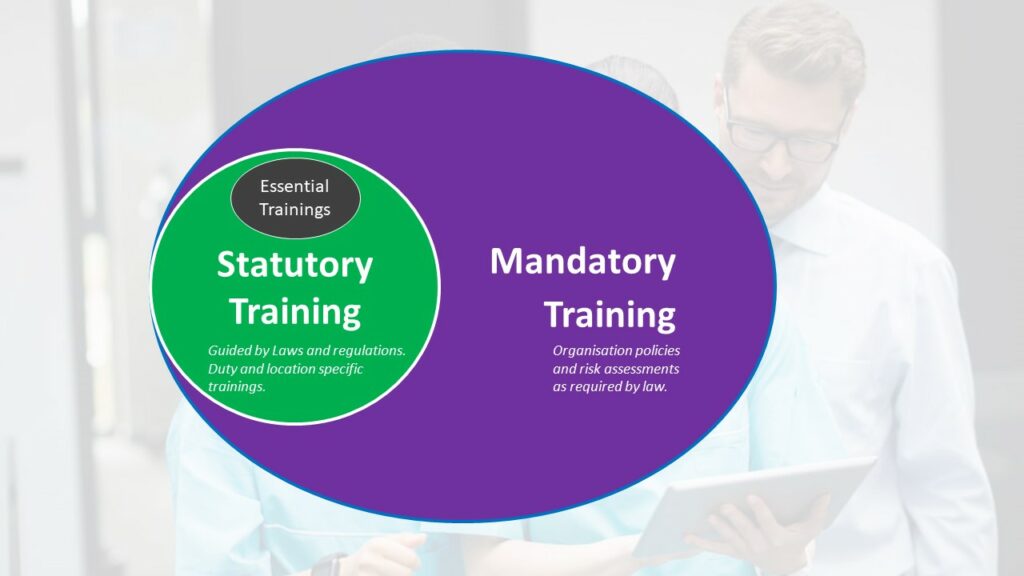
Statutory training refers to training that is required by specific laws and regulations. Mandatory training encompasses training required by organisational policies, risk assessments, and procedures. All statutory training would be considered mandatory, since organisations must comply with relevant laws.
But some additional training may be mandatory for a given role or workplace without being legally required for all healthcare providers.
Let’s first decode these two terms which are often used interchangeably:
Statutory Training:
Mandatory Training:
All statutory training is mandatory, but not all mandatory training is statutory.
Think Venn diagram with overlap. We’ll explore common examples shortly.
Leaders often get questions on why certain modules are deemed mandatory. Reasons include:
While mandating some learning seems burdensome, reasons like reducing harm make requirements worthwhile.
This refers to hands-on, practical courses focused on training needs with a statutory or legal mandate, as opposed to just theory or awareness.
Examples include practical sessions for manual handling, basic life support, infection control procedures, and fire safety response.
Employers must ensure healthcare professionals receive practical instruction and assessment on these critical risk areas per healthcare regulations.
While varying somewhat by specialty, typical required training modules cover:
Let’s explore some prominent examples in more detail.
Basic life support skills enable rapid response to breathing and cardiac arrests in that critical first few minutes before experts can come to help.
Required training ensures we can provide potentially lifesaving assistance when emergencies strike.
Common BLS training topics include:
Some healthcare professionals like doctors and nurses require more advanced life support training for interventions like medications and advanced airways.
But core skills like high-quality CPR make BLS training mandatory for all direct care providers.

A 2020 study by the NHS Improvement found that statutory training on fire safety can improve evacuation procedures and reduce the risk of fire-related incidents in healthcare settings.
Catastrophic facility fires remain one of the highest hazard risks in healthcare.
Mandatory fire training prepares us to contain fires, safely evacuate, and prevent their ignition in the first place.
Standard fire training instruction covers:
Fire drills applying learning in situ are key to responding instinctively when real emergencies strike.
Preventing the spread of infections protects both healthcare workers and vulnerable patients. Typical infection control modules include:
Reinforced hygiene habits like thorough hand washing between patients prevents countless transmissions.
Obtaining proper consent honors patient rights and promotes ethical care.
Key content areas are:
Getting really good at talking about consent stops misunderstandings that can go against what patients want and create problems.

A 2018 study by the Royal College of Nursing (RCN) found that mandatory training on medication administration can reduce medication errors by up to 30%.
FAQ: What is an example of statutory training?Some examples of training required by statute in healthcare settings include:
1. Fire safety training mandated under Regulatory Reform (Fire Safety) Order 2005.
2. Health and safety training required by Health and Safety at Work Act 1974.
3. Data protection and information governance training complying with Data Protection Act 2018.
4. Safeguarding training dictated by various child and vulnerable adult protection laws.
5. First aid training fulfilling the Health and Safety (First Aid) Regulations 1981.
While many modules are universal, certain designated training is mandated based upon roles:
Customised learning to environment and duties makes sure healthcare workers have the skills they need for their usual tasks and the challenges they might face.
Understanding expectations and receiving support to fulfill them enables learners to embrace requirements.
We recommend that a member of your team attends a specific train-the-trainer course to gain a better understanding of how to handle training for your organisation. This would provide a clear approach to developing and delivering effective training programs.
Well-crafted education experiences make mandated modules more motivating and sticky.
Thoughtful engagement strategies make mandated training feel more purposeful than passive.
Consistent compliance monitoring ensures training translates into practice:
What gets monitored gets managed. Gentle compliance nudges work better than penalties.
Classrooms must connect to clinical care to achieve outcomes:
Without support for integration into hectic workflows, concepts taught can too easily be forgotten.
Training overload demotivates rather than activates learning.
Principles to prevent training overload include:
While extensive, requirements can feel manageable when thoughtfully coordinated, formatted and delivered.
We hope this guide helps provide reassuring rationale for the safety and compliance training we undertake as healthcare professionals.
While burdensome at times on top of our duties, the shared goal of protecting patients ultimately makes requirements worthwhile.
We shoulder these obligations together for the greater good.
By embracing mandated training with grace and purpose, we elevate care quality, colleague support, and public trust in our noble profession.
Our learning truly lifts all when we recognise its deeper connections to safety and excellence.
For advice on training needs, please talk to our team 01782 563333 or send us an email: enquiries@caringforcare.co.uk.

A 2017 study by the National Health Service (NHS) England found that mandatory training on infection prevention and control (IPC) can reduce healthcare-associated infections (HAIs) by up to 50%.
Statutory requirements form a subset of overall mandatory training, so the terms are not fully interchangeable.
Think of mandatory as the larger umbrella encompassing all compulsory employer-required training.
The component that is legally required by specific regulations makes up statutory training.
So all statutory training is mandatory, but not all mandatory training is statutory.
What is statutory and mandatory training for care homes?Care homes have a range of core statutory and mandatory training requirements for their staff under CQC guidelines and health and safety laws.
Common subjects include safeguarding, mental capacity, infection control, moving and handling, food safety, fire safety, first aid, health and safety, medication management, and data protection.
Refresher frequencies are often set annually or every 3 years.
What is statutory and mandatory training in health and social care?Common statutory trainings cover fire safety, health and safety, first aid, safeguarding, Mental Health Act, Mental Capacity Act, deprivation of liberty, food safety, hazardous materials, and infection control.
The specific subjects and frequencies are dictated by laws like Health and Safety at Work Act, Food Safety Act, and data protection regulations.
We’ll help you find the right course for your needs. Tell us a little bit about your situation and what you would like to achieve.
We’ll get back to you within one working day.